By Philip Rotstein —
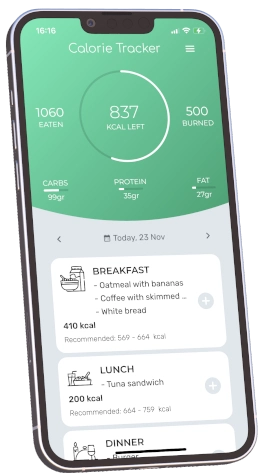
Simply cutting calories won’t work for PCOS. It’s a complex condition that demands a holistic approach, considering all aspects of your health. But there are effective ways to manage it.
In this article, we’ll move beyond calorie counting and offer practical tips to help you deal with PCOS and enhance your overall well-being.
Why Is It Hard To Lose Weight With Pcos?
Polycystic Ovary Syndrome (PCOS) is more than just a challenge; it’s a complex hormonal condition that has become a widespread concern, affecting a significant proportion of women worldwide.
At its core, PCOS involves an imbalance in reproductive hormones, creating a cascade of symptoms that can deeply impact a woman’s life.
One of the most visible and distressing of these symptoms is weight gain, often accompanied by insulin resistance – a condition where the body’s cells don’t respond effectively to insulin, leading to elevated blood sugar levels.
This insulin resistance not only exacerbates weight gain but also makes shedding those extra pounds an uphill battle.
The traditional weight loss advice – create a calorie deficit by consuming fewer calories than you burn – seems straightforward.
However, the question arises: does this approach hold water for individuals grappling with PCOS?
Given the unique metabolic and hormonal challenges posed by this syndrome, can a simple calorie deficit effectively lead to weight loss for those with PCOS?
This is not just a question of dieting efficacy; it’s about understanding a condition that defies conventional weight loss wisdom.
Trying to understand why is it so hard to lose weight with pcos, we discuss the complexities of PCOS and figure out whether the time-honored rule of calorie counting is a friend or foe in the battle against PCOS-related weight gain.
Understanding PCOS and Weight Gain
The Role of Hormonal Imbalances in PCOS
To fully grasp the weight management challenges faced by those with PCOS, it is crucial to understand the underlying hormonal imbalances that define this condition.
Insulin Resistance and Its Impact
Central to PCOS is insulin resistance, a state where the body’s cells become less responsive to insulin, the hormone responsible for regulating blood sugar levels.
This resistance leads to higher circulating insulin levels, which not only exacerbate the risk of developing diabetes but also contribute to weight gain.
Insulin, in excess, promotes belly fat storage, particularly in the abdominal area, making weight loss more challenging for those with PCOS.
Inflammation - A Key Player in PCOS
In addition to insulin resistance, inflammation plays a pivotal role in PCOS.
Chronic low-grade inflammation, commonly observed in PCOS, further disrupts hormonal balance and exacerbates insulin resistance.
This inflammatory state can be both a cause and a consequence of weight gain, creating a vicious cycle that’s hard to break.
Beyond Caloric Intake: Understanding PCOS-Related Weight Gain
This complex interplay of hormonal imbalances is often a more significant contributor to weight gain in PCOS than excessive calorie intake.
While overeating can contribute to weight gain in any individual, in PCOS, it’s the hormonal milieu that predominantly drives the weight increase.
The Limitations of Calorie Counting in PCOS
This reality brings to light a critical oversight in the conventional approach to weight loss: calorie counting may not be enough.
Why Calorie Counting Falls Short
Calorie counting, the traditional method of weight management, focuses primarily on the energy equation — calories in versus calories out.
However, this method can be overly simplistic when it comes to PCOS.
By concentrating solely on calories, we may neglect the hormonal aspects of PCOS, which are integral to understanding and effectively managing weight.
A Call for a More Nuanced Approach
This one-dimensional approach overlooks the fact that for individuals with PCOS, it’s not just about how much they eat, but also about how their bodies respond to these foods on a hormonal level.
Hence, a more nuanced approach that takes into account these hormonal dynamics is essential for effective weight management in PCOS.
The Limitations of Calorie Deficit in PCOS
The Downside of Calorie Counting in PCOS
The practice of calorie counting, widely endorsed as a universal solution for weight loss, runs into several roadblocks when it comes to managing PCOS. This approach, while straightforward in theory, fails to account for the nuanced complexities of PCOS, leading to potential negative outcomes.
Overlooking Nutritional Quality
“ This holistic approach to nutrition is essential with PCOS ”
One of the significant pitfalls of calorie counting in PCOS is its tendency to sideline the quality of nutrition. This method focuses on the quantity of calories consumed, often at the expense of the nutritional value of the food.
For individuals with PCOS, the type of food—rich in nutrients, low in processed sugars, and inflammation-reducing—is as important as the caloric content.
This holistic approach to nutrition is essential for managing insulin resistance and hormonal imbalances, core aspects of PCOS that are not addressed by simply counting calories.
Risks of Disordered Eating
Calorie counting can also pave the way for disordered eating behaviors. The obsessive focus on numbers and strict dietary control can lead to an unhealthy relationship with food, particularly in women with PCOS who may already be struggling with the psychological impacts of their condition. The stress and anxiety surrounding food choices and calorie intake can exacerbate PCOS symptoms, creating a counterproductive cycle.
The Stress of Dietary Restrictions
Moreover, the stress associated with rigorous calorie counting and food restrictions can have its own set of consequences.
Stress is a known factor in exacerbating PCOS symptoms, including weight gain.
The mental and emotional burden of constantly measuring and restricting food intake can lead to elevated cortisol levels, further impeding weight loss efforts in those with PCOS.
Inadequacy of Traditional Calorie Reduction Advice
The conventional wisdom of creating a calorie deficit through dieting does not take into account the unique challenges faced by individuals with PCOS.
This one-size-fits-all approach disregards the hormonal intricacies and metabolic peculiarities inherent to this condition.
Hormonal Complexities in PCOS
PCOS is characterized by a complex hormonal imbalance, including elevated androgens, insulin resistance, and often, chronic inflammation.
These factors contribute to weight gain and make losing weight more challenging than in individuals without PCOS. A simple reduction in caloric intake does not address these hormonal disturbances, which are key drivers in the weight management struggles of those with PCOS.
The Need for a Tailored Approach
Given these complexities, it becomes clear that a more tailored approach is necessary for effective weight management in PCOS.
Strategies that go beyond calorie counting and address the hormonal and physiological nuances of the condition are essential.
This includes focusing on the types of foods consumed, the timing of meals, and the inclusion of lifestyle changes that collectively address the hormonal imbalances, insulin resistance, and inflammatory processes inherent in PCOS.
In summary, while calorie deficit strategies may work for the general population, their effectiveness is limited when applied to the unique context of PCOS.
Understanding and addressing the hormonal and physiological factors at play is crucial for devising an effective weight management strategy for those living with this condition.
Practical Steps and Strategies
To tailor a path that respects both the condition and the individual, we must consider specific dietary choices, physical activities, and lifestyle changes. Additionally, understanding one’s unique physiological state through medical tests is crucial in crafting a personalized management plan.
Tailored Dietary Choices and Physical Activity
Nutritional Strategies for PCOS
For dietary modifications, the focus should be on foods that aid in balancing blood sugar and reducing inflammation, two key aspects of PCOS.
A diet rich in:
- whole foods,
- lean proteins,
- healthy fats,
- and fiber
can help manage insulin levels and hormonal imbalances. Incorporating foods like leafy greens, nuts, seeds, and lean meats, while limiting processed sugars and high-glycemic index foods, is advisable.
In terms of physical activity, a combination of cardio and strength training can be beneficial. Regular exercise helps improve insulin sensitivity and can aid in weight management. It’s important to choose activities that are enjoyable and sustainable in the long run.
The Role of Supplements
Certain supplements can also play a supportive role in managing PCOS. For instance, inositol, omega-3 fatty acids, and magnesium have been shown to help with insulin resistance and hormonal balance. However, supplements should be chosen based on individual needs and preferably under the guidance of a healthcare professional.
The Importance of Medical Testing
Understanding the specific hormonal and metabolic imbalances is key in PCOS management.
Tests for DHEAs, Free Androgen Index (FAI), fasting insulin, and glucose levels provide valuable insights.
These tests can help identify individual needs and tailor strategies for dietary choices, supplementation, and lifestyle modifications.
Balancing Blood Sugar and Reducing Inflammation
Maintaining blood sugar balance is pivotal in managing PCOS. This involves not just what you eat but also when and how often you eat. Small, frequent meals with a balance of protein, fat, and carbohydrates can help stabilize blood sugar levels throughout the day.
Addressing inflammation through diet is equally important.
An anti-inflammatory diet that includes foods like fatty fish, turmeric, ginger, and berries can be beneficial.
Reducing the intake of inflammatory foods, such as processed foods, sugars, and certain fats, is also crucial.
Realistic Expectations and Long-Term Management
Managing expectations is important in the journey of PCOS management. Weight loss and hormonal balance are not overnight achievements. Setting realistic goals, understanding that progress may be slow, and acknowledging that setbacks can occur is essential.
Long-term management of PCOS involves a commitment to lifestyle changes and regular monitoring of one’s health status. It’s not just about a short-term diet or exercise regimen; it’s about a sustainable lifestyle that accommodates the needs and challenges posed by PCOS. This holistic approach, encompassing dietary changes, physical activity, stress management, and medical support, is key to effectively managing PCOS over the long term.
Realistic Expectations and Long-Term Management
In the journey of managing PCOS, setting realistic expectations is a cornerstone of success.
Recognizing that weight loss and hormonal balance in PCOS are gradual processes is vital.
This approach underscores the importance of sustainable progress rather than rapid transformations.
It’s crucial to understand that small, consistent changes over time are more beneficial than drastic, short-lived diets or exercise fads.
Addressing the Psychological Aspects
The psychological aspects of weight management in PCOS cannot be overstated.
Stress reduction is essential, as stress can exacerbate PCOS symptoms, including weight gain.
Techniques such as mindfulness, meditation, and yoga can be instrumental in managing stress levels.
Additionally, cultivating a healthy relationship with food is critical.
This involves moving away from viewing food as an enemy and embracing it as nourishment and a source of joy.
It’s about creating a balanced approach to eating that is neither restrictive nor permissive but respects the body’s needs.
Debunking Myths and Quick Fixes
The diet industry is rife with myths and quick-fix promises, especially concerning PCOS and weight loss. It’s important to debunk these myths and understand that there is no one-size-fits-all solution for managing PCOS. Fad diets and rapid weight loss programs often fail to address the underlying issues of PCOS and can even be harmful in the long run. Sustainable lifestyle changes, tailored to individual needs, are the most effective way to manage PCOS.
Conclusion
In conclusion, while the traditional calorie deficit approach may work for the general population, it has significant limitations when applied to PCOS.
The hormonal and metabolic complexities of this condition require a more nuanced and holistic approach.
An effective strategy for managing PCOS involves understanding and addressing the hormonal imbalances, insulin resistance, and inflammation that are central to this condition.
It is crucial for individuals with PCOS to seek personalized advice and support.
This might involve consulting healthcare professionals who specialize in PCOS, joining support groups, or engaging in communities that offer shared experiences and knowledge.
Managing PCOS is not just about dealing with the physical symptoms but also about empowering oneself with the right information and support.
As we conclude, it’s important to leave you with a message of empowerment.
Living with PCOS is undoubtedly challenging, but it is also manageable. With the right approach, support, and knowledge, individuals with PCOS can lead healthy, fulfilling lives.
Remember, managing PCOS effectively is not just about overcoming its symptoms; it’s about embracing a lifestyle that fosters well-being, balance, and personal growth.
Research sources
- Overview of literature on weight management strategies in women with PCOS.
- Discusses the implications of weight gain and obesity on PCOS and how weight loss improves PCOS features.
- A study on the specific weight management practices used by women with PCOS and their impact.
- Focuses on the importance of weight management as a key component of treatment for women with PCOS and coexistent obesity.
- A review of studies describing hormonal, metabolic, and weight effects of different weight loss strategies for adolescents with PCOS.
- Explores the broader aspects of lifestyle management in PCOS, including diet and behavioral management.
- Recommendations for a balanced diet and optimum physical activity to reduce severe PCOS symptoms and improve metabolic balance.
- An extensive narrative review of lifestyle modifications for women with PCOS.
- Discusses the role of the ketogenic diet in PCOS management, particularly its effects on hormonal balance.
- Focuses on lifestyle management as the first-line treatment for improving PCOS complications and the challenges women face in implementing these changes.